
48 ISE Magazine | www.iise.org/ISEmagazine
Improving patient treatment,
satisfaction at a small hospital
Monroe County Hospital is a critical access hospital located in
Forsyth, Georgia. It is a 25-bed facility comprising an emer-
gency department (ED) and medical-surgical unit that cares for
inpatient and rehabilitation patients. The ED sees just over 8,500
patients annually from six counties in middle Georgia. This hos-
pital has been providing access to high quality health services to
the citizens of Monroe County since 1954 when the hospital au-
thority was founded (monroehospital.org/about/history-and-mission.
cms).
In 2016, this facility became a strategic partner of Navicent
Health based in Macon, Georgia. In 2018, Monroe County Hos-
pital became DNV GL accredited and was on track to become
ISO 9001:2015 certified this spring. In 2019, the team embarked
on the high-performance journey in the spirit of continuous im-
provement. As part of the certification process, the leadership
team set out to identify and eliminate any and all types of waste
plaguing the hospital’s operational environment.
These initial efforts focused on delays in the emergency de-
partment wait times. This is significant because such delays un-
favorably impact quality of care, revenues and customer satisfac-
tion levels when patients leave without treatment. The ultimate
goal was to provide safer and more effective care to all patients.
The team was sponsored by the CEO, who is an IISE-trained
Black Belt, along with other leaders. The project was initiated
in January 2019 and concluded December 2019. But outcomes
are still monitored and adjustments made as needed to ensure
“wins” are sustained long term. The team used a standard DMA-
IC methodology to define the problem, measure the current state,
analyze the data, improve the noted issues and control the changes
long term. Moreover, many cross-functional stakeholders were
included in the process to ensure the improvements were maxi-
mized, sustained and culturally adopted.
The process, project and outcomes
Define. Extended wait times and subsequent alarm about pa-
tients who leave emergency departments without treatment has
become a mounting national concern. In January 2019, the proj-
Solutions in practice by Chasatie Whitley,
Casey Fleckenstein, Lorraine Smith, Hershel
Kessler and Casey Bedgood
case study

May 2021 | ISE Magazine 49
case study
ect team developed and implemented a method to decrease
wait times and thus the number of patients who left with-
out being treated (LWOT). According to the Community
Health Needs Assessment of 2016, access to care was iden-
tified as a need in our community. The team interpreted
that the low ED volume, increased wait times and increased
LWOT rates indicated that patients were seeking emergen-
cy treatment elsewhere in our region. This decreases their
access to care within the community and unfavorably im-
pacts revenues.
The focus of the project was on reducing LWOTs in the
emergency room. These patients are an issue for a variety
of reasons. First, delays in care represent waste and result
in patients seeking treatment at alternate care sites. This
inhibits access to care, reduces quality of care and nega-
tively impacts patient satisfaction and revenues. Moreover,
if customers cannot receive services when, where and how
they desire them, the hospital’s reputation will be less than
favorable.
The goal of the project was to initially reduce LWOTs
monthly to the national benchmark of 2% or less (Medicare.
gov, 2018). Long term, the ideal goal was zero LWOTs each
day. Unfortunately, the rate for Monroe County Hospital
was over 2% on average in 2018. Also, the team focused on
increasing patient satisfaction levels to the national bench-
mark. The initial goal was 75% favorable each month.
It’s important to note that if goals are not consistently
achieved, volumes, quality of care, customer satisfaction
and revenues will continue to decline. Moreover, the pub-
lic’s perspective of the organization would be further im-
pacted.
Measure. The main key performance indicators chosen
by the team were monthly LWOT rates and patient satis-
faction scores (percent favorable). The desired trend is to
achieve fewer LWOTs and higher patient satisfaction scores
each month. Both metrics were measured monthly over a
year before the project began. Post project, the results were
measured monthly for over a year as well to ensure the sus-
tainment of wins. Figure 1 shows performance to goal for
both metrics before the project showing that patient sat-
isfaction scores were meeting goal only 20% of the time.
The LWOT scores were only meeting goal 47% of the time
pre-project for the same time period.
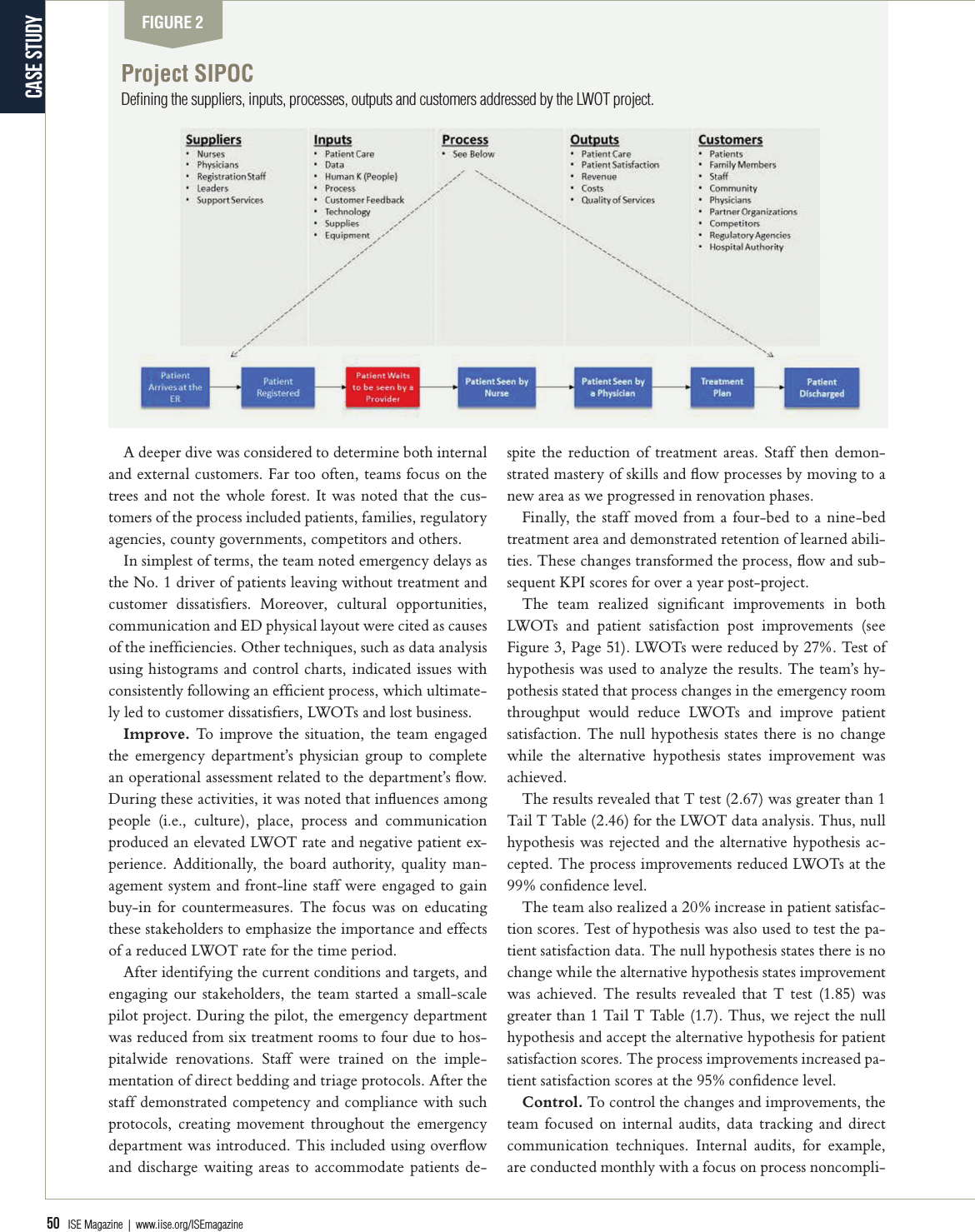
Analyze. To analyze the current state, the team started
with a high-level process map (i.e., SIPOC; shown in Figure
2, Page 50). The team used the SIPOC to identify the suppli-
ers, inputs, process, outputs and customers of the ED process.
The suppliers represented various stakeholders ranging from
leadership to front-line staff. These stakeholders would be
crucial in addressing the waste and inefficiencies. The inputs
related to items such as people, training, data, equipment and
more. The outputs were very straightforward: clinical care,
quality, revenue and customer satisfaction.
FIGURE 1
Pre-project KPI graphs (actual versus goal)
Performance metrics before the project showed that patient satisfaction scores and patients leaving without treatment numbers were below
the goals set.
Leaders must measure, track and know
their organization’s numbers. Data is
like a sheet of music that will tell you
exactly where the problem is when you
know how to interpret it.
50 ISE Magazine | www.iise.org/ISEmagazine
case study
A deeper dive was considered to determine both internal
and external customers. Far too often, teams focus on the
trees and not the whole forest. It was noted that the cus-
tomers of the process included patients, families, regulatory
agencies, county governments, competitors and others.
In simplest of terms, the team noted emergency delays as
the No. 1 driver of patients leaving without treatment and
customer dissatisfiers. Moreover, cultural opportunities,
communication and ED physical layout were cited as causes
of the inefficiencies. Other techniques, such as data analysis
using histograms and control charts, indicated issues with
consistently following an efficient process, which ultimate-
ly led to customer dissatisfiers, LWOTs and lost business.
Improve. To improve the situation, the team engaged
the emergency department’s physician group to complete
an operational assessment related to the department’s flow.
During these activities, it was noted that influences among
people (i.e., culture), place, process and communication
produced an elevated LWOT rate and negative patient ex-
perience. Additionally, the board authority, quality man-
agement system and front-line staff were engaged to gain
buy-in for countermeasures. The focus was on educating
these stakeholders to emphasize the importance and effects
of a reduced LWOT rate for the time period.
After identifying the current conditions and targets, and
engaging our stakeholders, the team started a small-scale
pilot project. During the pilot, the emergency department
was reduced from six treatment rooms to four due to hos-
pitalwide renovations. Staff were trained on the imple-
mentation of direct bedding and triage protocols. After the
staff demonstrated competency and compliance with such
protocols, creating movement throughout the emergency
department was introduced. This included using overflow
and discharge waiting areas to accommodate patients de-
spite the reduction of treatment areas. Staff then demon-
strated mastery of skills and flow processes by moving to a
new area as we progressed in renovation phases.
Finally, the staff moved from a four-bed to a nine-bed
treatment area and demonstrated retention of learned abili-
ties. These changes transformed the process, flow and sub-
sequent KPI scores for over a year post-project.
The team realized significant improvements in both
LWOTs and patient satisfaction post improvements (see
Figure 3, Page 51). LWOTs were reduced by 27%. Test of
hypothesis was used to analyze the results. The team’s hy-
pothesis stated that process changes in the emergency room
throughput would reduce LWOTs and improve patient
satisfaction. The null hypothesis states there is no change
while the alternative hypothesis states improvement was
achieved.
The results revealed that T test (2.67) was greater than 1
Tail T Table (2.46) for the LWOT data analysis. Thus, null
hypothesis was rejected and the alternative hypothesis ac-
cepted. The process improvements reduced LWOTs at the
99% confidence level.
The team also realized a 20% increase in patient satisfac-
tion scores. Test of hypothesis was also used to test the pa-
tient satisfaction data. The null hypothesis states there is no
change while the alternative hypothesis states improvement
was achieved. The results revealed that T test (1.85) was
greater than 1 Tail T Table (1.7). Thus, we reject the null
hypothesis and accept the alternative hypothesis for patient
satisfaction scores. The process improvements increased pa-
tient satisfaction scores at the 95% confidence level.
Control. To control the changes and improvements, the
team focused on internal audits, data tracking and direct
communication techniques. Internal audits, for example,
are conducted monthly with a focus on process noncompli-
FIGURE 2
Project SIPOC
Defining the suppliers, inputs, processes, outputs and customers addressed by the LWOT project.

May 2021 | ISE Magazine 51
If you’ve been involved in a project that put solutions to the test in a
real-world environment, it could be a potential Case Study article. Please
send your idea to Managing Editor Keith Albertson at kalbertson@iise.org
for consideration.
Do you have a Case Study to share?
ance. These teams journey to the gemba, where the work
happens, to assess if processes are being followed consistent-
ly. If issues are noted, the respective leaders must initiate
a corrective action plan immediately for resolution. Then,
teams reaudit to ensure corrections were successful.
Second, the team tracks data monthly for all KPIs against
national benchmark goals. If goals are not attained, the data
is communicated to senior leaders, the board and quality
management system for magnification and resolution.
Finally, both vertical and horizontal communication
techniques are used to ensure all stakeholders are apprised
of and track the current environment. If changes are need-
ed, the goal is to make interventions in real time when
possible.
Lessons learned
There are several pearls the team learned from the project.
First, the voice of the customer is always a great starting point
for any improvement project. Always focus on the customer
and be able to answer: What do they want, need and expect
from the organization? If gaps exist, teams should focus on
measuring, validating and correcting the gaps.
Second, leaders must measure, track and know their or-
ganization’s numbers. Data is like a sheet of music that will
tell you exactly where the problem is when you know how
to interpret it. The team learned that it’s better to initiate
data-driven interventions sooner than later.
Third, the gemba should always be a focal point when
solving process-related issues. Go to where the work is be-
ing done, talk to those closest to the process to understand
the issues and incorporate those at the gemba in the solution
process.
Finally, there is no substitute for a good process. Good
processes or lack thereof can make or break an organiza-
tion, particularly in healthcare. The team learned that
starting with a sound, data-driven process, measuring the
process outcomes regularly, auditing the process routinely
(not just the activities being performed) and real-time cor-
rections of nonconformities are paramount in meeting and
exceeding customer requirements.
Chasatie Whitley, BSN, RN, CEN, is process owner for Navi-
cent Health.
Casey Fleckenstein, BSN, RN, is nurse director and an IISE-
trained Lean Six Sigma Green Belt for Navicent Health.
Lorraine Smith, MBA, MT(ASCP)SH, is CEO, executive
sponsor and an IISE-trained Black Belt. Contact her at Lorraine.
Smith@atriumhealth.org.
Hershel Kessler, DO, is emergency department medical director for
Navicent Health.
Casey Bedgood, MPA, CSSBB, is the system accreditation op-
timization officer at Navicent Health and an IISE-trained Lean
Green Belt, Six Sigma Green Belt and Six Sigma Black Belt. He
was an adviser and Black Belt sponsor for this project. He is an
IISE member.
FIGURE 3
Postproject KPI improvements
Results show significant improvements in the number of patients leaving without treatment (down 27%) and increased patient satisfaction.
